Summary of the AMA Digital Health Implementation Playbook and implications for the Pharmacy Profession
The AMA has a Playbook for Digital Health
And yet where is the pharmacy profession?
The American Medical Association (AMA) has not been silent compared to other medical organizations around its views on digital health. They have had an open discourse in the past year and partnered with many outside organizations to quantify and assess the implications of the digital health space in medical practice. If you were not aware (or a part of), the AMA has had several open networks inciting discussions and joint thoughts on digital health and established a digital health leadership program.
As part of this program, there has been an interest in delivering care using digital health, with a focus on Validation & Evidence, Payment, Liability & Risk, and Adoption & Scale. While these may be ambivalent terms, the AMA has put its word into more action with their recently released "Digital Health Implementation Playbook" (you can download it here but will need to submit some user data). I have read this document a few times and reflected on its implications to practice, which I will detail henceforth.
The Playbook is 95 pages long, and 66 pages actually dedicated towards essential content with the remainder being ancillary supporting documents and tools to integrate into clinical use. Overall, a lot of the material is image and graph-heavy, with not a lot of actual text, and with many quotes and such thrown in. I would say perhaps if they just stuck with actual text like a whitepaper this thing may only be <30 pages in actual content. The document is broken into four parts:
Part 1 - Warmup
The playbook starts with an introduction to digital health and the significance of the document. The AMA focuses on the four key requirements they feel, including:
Does it work?
Will I receive payment?
Will I be liable?
Will it work in my practice?
These items are similar to what they have highlighted in their leadership page, so comes as no surprise. I would say for anyone that is familiar with Digital Health, and part one really reveals nothing significant. Instead, the only thing to take away would be that they explain their focus on Remote Patient Monitoring as one of the critical areas, to begin with using digital health solutions, and the target clinical area of hypertension management. This then, in turn, leads into the following two parts: "Pre-Game" and "Game Time."
Part 2 - Game Time
The second part is split into six steps that detail how to get ready to implement a digital health practice solution.
Identifying a Need
Essentially identifying where in a health system or organization that a digital health solution would be beneficial. The key takeaway would be what needs to be improved and using technology for that area, which I take to reinforce people to stop grabbing random tech and just trying to figure out where to squeeze it in. One area I thought that was cool was the focus on end-users to get buy-in for implementation of a program.
Forming a Team
This goes without saying, but a good team is needed to get any project off the ground and rolling along. The appendix lists such players, including core members, leadership, advisors and implementation members.
Defining Success
Essentially create what the end goals of the program or service will be, and how to stick to them. The appendix includes a S.M.A.R.T checklist to follow along with. I did enjoy their mention that it is essential to keep in mind the global picture of what is trying to be accomplished instead of focussing on just one step at a time.
Evaluating the Vendor
I really think this is a crucial point to make, and while the previous three steps are generally good business/project practice, this part stands out. I mean, yes, many organizations have experience picking up technology hardware or software to utilize with one of the most significant examples being and EHR platform, but Digital Health is a bit different. You have to question the evidence of a platform, the scale of the service, sustainability of the product, etc. This is perhaps one of the best sections in Part 2 of the AMA playbook.
Making the Case
Essentially doing all the groundwork then making a proposal to the organization to get a rollout and getting the overall organization and members on board.
Contracting
Really nothing surprising here.
Summary of Part 2
Overall, nothing groundbreaking in this section, just good advice. I feel the focus on finding a vendor the best part of this area and one that ancillary supporting documents in the appendix can help with.
Part 3 - Game Time
This section details the implementation part of Part 2 work, with a focus on Remote Patient Monitoring (RPM). I think this has the best tidbits to show how to roll out a digital health enabled service and will indeed be the essential part of the AMA playbook. I expect the playbook to be updated over time with other areas, but honestly, RPM is probably the easiest and lowest stake to get into, especially considering upcoming changes to billing codes by CMS focused on RPM in 2019 which I suspect everyone is keeping an eye on.
Designing the Workflow.
YES. I am a huge proponent of a streamlined workflow, and I see digital health really being a wrench thrown into the gears of clinical workflow that has overall remained mostly unchanged for quite some time (which is based on the current environment of digital health not being fully integrated into EHRs, use of outside platforms, and patient responsibility of technology use). Perhaps one of the most significant takeaway points was to streamline the workflow to maximize the patient experience and get the best data possible for collection to be clinically analyzed. However, one of the areas I thought most interesting (probably based on my profession) was the statement "Protect physicians from an overwhelming influx of data," which I believe goes beyond this group to all healthcare professionals. In any event, integration into the EHR is critical - and any vendors reading this will want to make sure that is their priority if not already accomplished as I feel it will make or break any company in the future.
Preparing the Care Team
Goes without saying, but no technology should just be dropped on a healthcare team suddenly. I mean, if you have been part of an EPIC EHR rollout you know what I am talking about, it's a serious endeavor. This may be slightly less intense, but you want all users ready to hit the ground running and have buy-in to the service. Maintaining clear communication and feedback from the team will be key.
Partnering with the Patient
In the era of the E-Patient movement, I feel this needs to be a step. The patient as a consumer is a growing mentality, and they need to be empowered and enabled to use this technology in their care. It's one thing to throw a device at them to collect data, but a more significant movement to show them why it is essential. I would say this has been my biggest argument why so many early (and current) studies in the digital health space have failed as many interventions seem tech-heavy and less patient focused. After all, it's another tool they will have to be adherent to have any clinical utilization in practice. Perhaps one item that stood out to me was the one section on identifying patients 'likely to succeed' which I found interesting.
Implementing
Basically launching whatever program is developed and making sure all goals set out in Part 2 are met.
Evaluating Success
Similarly, tracking what measurements you had established to quantify and return to your leadership or organization committees that the project is working.
Scaling
Going beyond what you just did and avoiding a 'Pilot Graveyard.'
Part 3 Summary
Overall, I would say the first few parts are critical in the workflow and team building needed to get the program running, but analyzing what you are doing to ensure success can't be glossed over.
Part 4 - Post Game
Essentially the appendix with resources and documents relevant to Part 2 & 3 steps covered. Some may be more useful than others, but perhaps for an inexperienced team or organizations, it will at least be a good starting point.
My Takeaway Points and Implications for Pharmacy Practice
When I saw this document, I was really impressed and envious of what the AMA got going with all the collaboration it undertook to create this playbook. I had been giving several CE and national talks, and one of my focus areas have been in ways pharmacists can use digital health to expand clinical services.
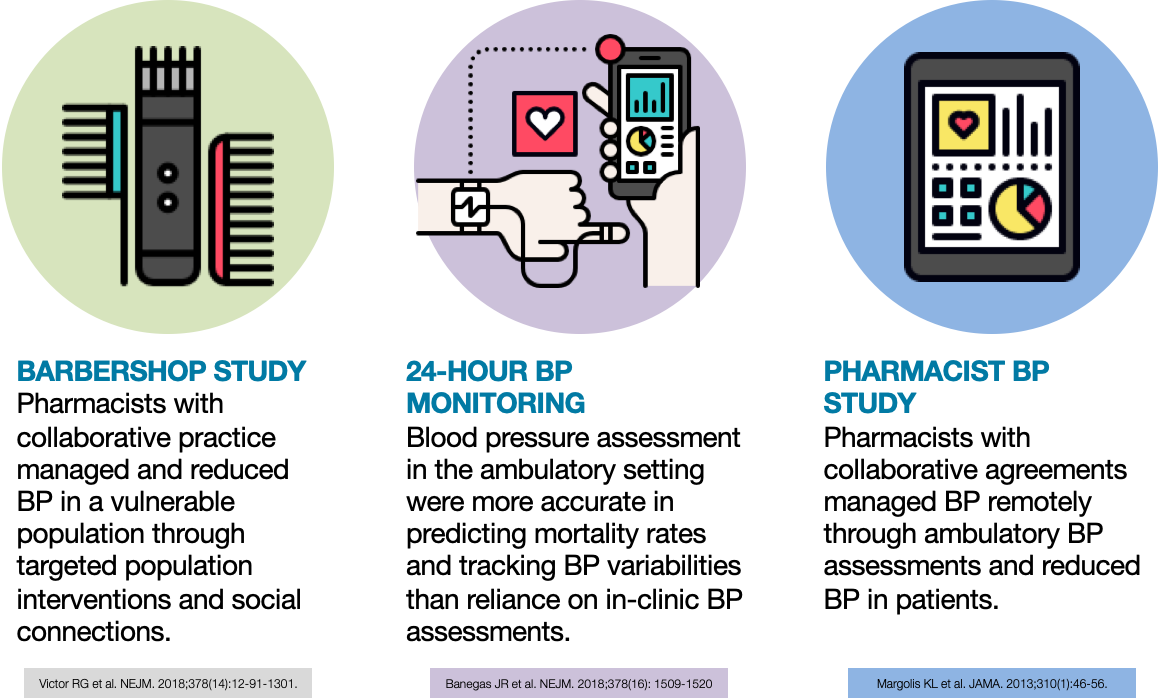
One area that I have focused on has been RPM. My three/four studies I point out are the Barbershop Study, BP measurement study, and Telemanagement service run by pharmacists for hypertension management. Amazingly, the AMA directly point to the follow-up study published in 2018 on RPM of blood pressure by pharmacists as one of the key case studies of RPM in the playbook.
This is almost a slap in the face to a certain extent as it is not really discussed much in the playbook to utilize pharmacists in this way, but why should that be a focus, it's the AMA. Instead, I think organizations like ASHP and APhA should see this and ask themselves, why aren't we pushing for RPM billing as well? This has been a talking point, but I think we need to get some stake in the digital health environment and this is also our ticket in.
Take for instance the amount of tech out there that we could use for RPM of medication use and safety/efficacy beyond hypertension. We have a huge opportunity because the technology is there. We just need to make a profitable endeavor, and we need the support to get there.
As always, I welcome your thoughts!